How to strengthen iliopsoas for dance
The Muscle That Separates The Good From The Great…The Iliopsoas! – Feis Fit
Hey Dancers!
Today I’m going to talk about one of my absolute favorite muscles: the iliopsoas!!! I know, it sounds weird to be filled with enthusiasm about an odd sounding muscle but hear me out. Why do I love this muscle so much??! Well, a strong, flexible, and properly utilized iliopsoas separates excellent Irish Dancers from the mediocre. Google any ballet or gymnastics conditioning program and you will tons of information on the importance of engaging the iliopsoas because it is the MAIN muscle that is involved in hip flexion above 90 degrees (a.k.a: lifting your leg above parallel)! In addition to helping get your kicks and clicks high, the iliopsoas:
-Works as a stabilizer in maintaining proper alignment (aka: good posture).
-Enables your body through proper posture to utilize muscles in your glutes and deep outward rotators (butt muscles and turnout muscles) to perform with more power and precision.
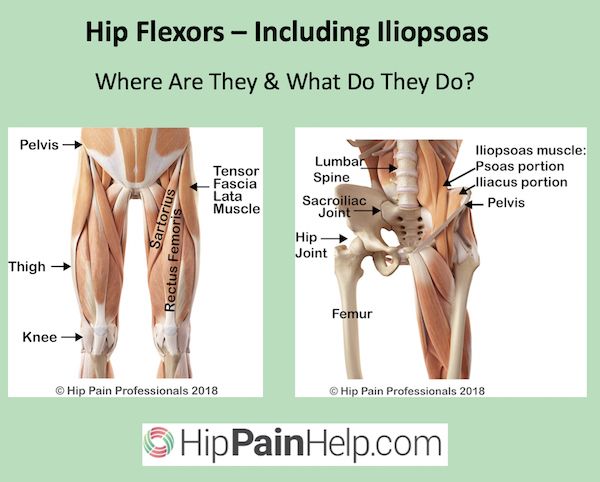
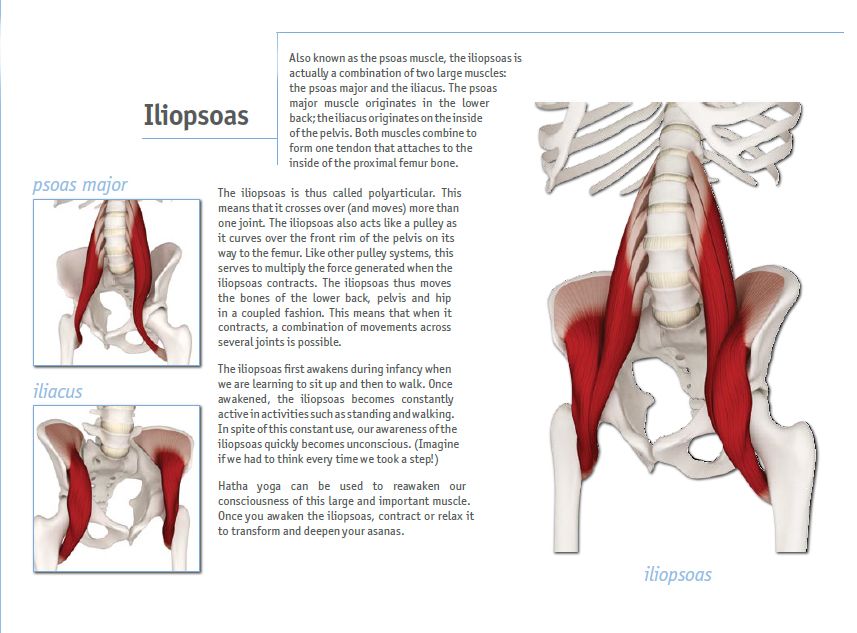
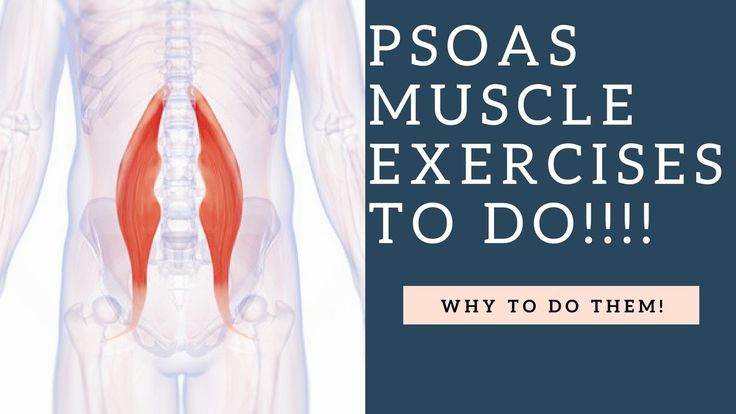
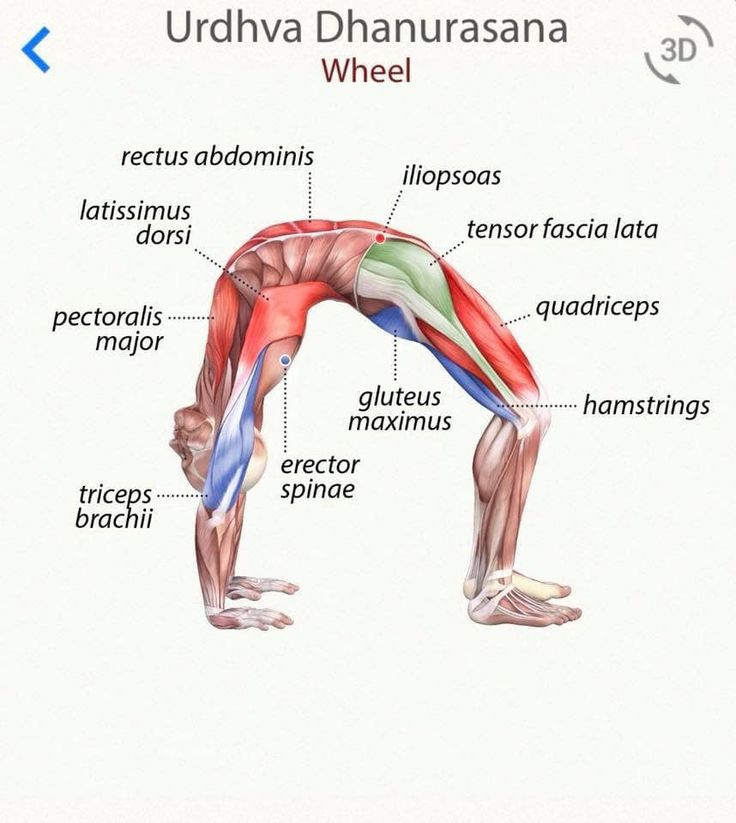
Improved power, turnout, posture, and higher kicks all with improving the strength and flexibility of one muscle?! Where can I sign-up?! And why isn’t this muscle talked about more in the Irish Dance world?! Truth is, this muscle is often forgotten because it is not visible. It’s easy to see if someone has crazy toned calves or quads but the illiopsoas is located deep deep deep in your midsection. The iliopsoas is actually a combination of three muscles: the iliacus, the psoas major, and the psoas minor, but all of these work together as the main hip flexor (leg lifter) so they are regularly referred to as one name, the iliopsoas. The muscle starts at the lower back and continues down to the top of your thigh bone. It is one of the only muscles that connects your upper body to your lower limbs hence why it is of the utmost importance to learn how to use!
Have you ever felt like you have hit a kick or click height plateau? No matter how long you have been working on your splits or stretching out after class, you just can’t seem to get your kicks ANY HIGHER? I was at a Feis this weekend and noticed low kicks/clicks to be a very common trend in the Open Championship competition. There were girls who were barely getting their kicks/clicks over parallel while appearing to be putting in maximal effort, meanwhile the girls who were able to get more height appeared to be doing it very naturally. So how is that some dancers can appear to effortlessly kick their legs up with great sharpness while others seem to get “stuck” with a leg at shoulder height? Common sense tells us that the dancer with lower kicks just needs to “stretch more,” but the truth is that it doesn’t matter how flexible you are, if you do not have a strong ilipsoas to bring your knee closer to your chest. If you do not learn how to strengthen and stretch your ilipsoas, you will never be able to get your kicks/clicks up while maintaining good posture. Why? As I mentioned before, the iliopsoas is the MAIN MUSCLE that works to bring the leg up after it passes parallel. Dancers will often try to use the quads and hamstrings to pull the leg up by tightening them. This can lead to that “stuck” leg feeling because squeezing the muscles close to the hip-joint will do exactly that: tighten the muscles around the hip socket, making the body work against itself in allowing the bone in the hip joint to move freely upwards above shoulder height.
There were girls who were barely getting their kicks/clicks over parallel while appearing to be putting in maximal effort, meanwhile the girls who were able to get more height appeared to be doing it very naturally. So how is that some dancers can appear to effortlessly kick their legs up with great sharpness while others seem to get “stuck” with a leg at shoulder height? Common sense tells us that the dancer with lower kicks just needs to “stretch more,” but the truth is that it doesn’t matter how flexible you are, if you do not have a strong ilipsoas to bring your knee closer to your chest. If you do not learn how to strengthen and stretch your ilipsoas, you will never be able to get your kicks/clicks up while maintaining good posture. Why? As I mentioned before, the iliopsoas is the MAIN MUSCLE that works to bring the leg up after it passes parallel. Dancers will often try to use the quads and hamstrings to pull the leg up by tightening them. This can lead to that “stuck” leg feeling because squeezing the muscles close to the hip-joint will do exactly that: tighten the muscles around the hip socket, making the body work against itself in allowing the bone in the hip joint to move freely upwards above shoulder height.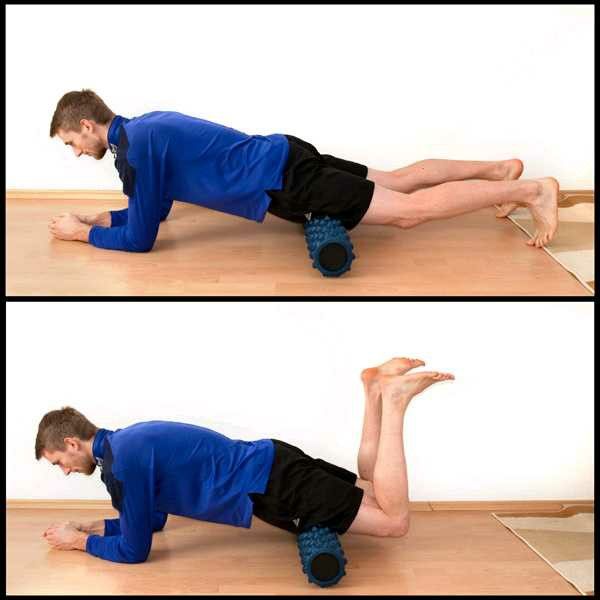 Thus the dancer is putting in tons of effort into having the body work AGAINST itself. The dancers who are appearing to kick effortlessly sky-high are able to keep their quads and hamstrings more relaxed (obviously not totally relaxed because the leg still needs to be straight) because they are using their iliopsoas in their core to “lift” rather than the quad to “pull.”
Thus the dancer is putting in tons of effort into having the body work AGAINST itself. The dancers who are appearing to kick effortlessly sky-high are able to keep their quads and hamstrings more relaxed (obviously not totally relaxed because the leg still needs to be straight) because they are using their iliopsoas in their core to “lift” rather than the quad to “pull.”
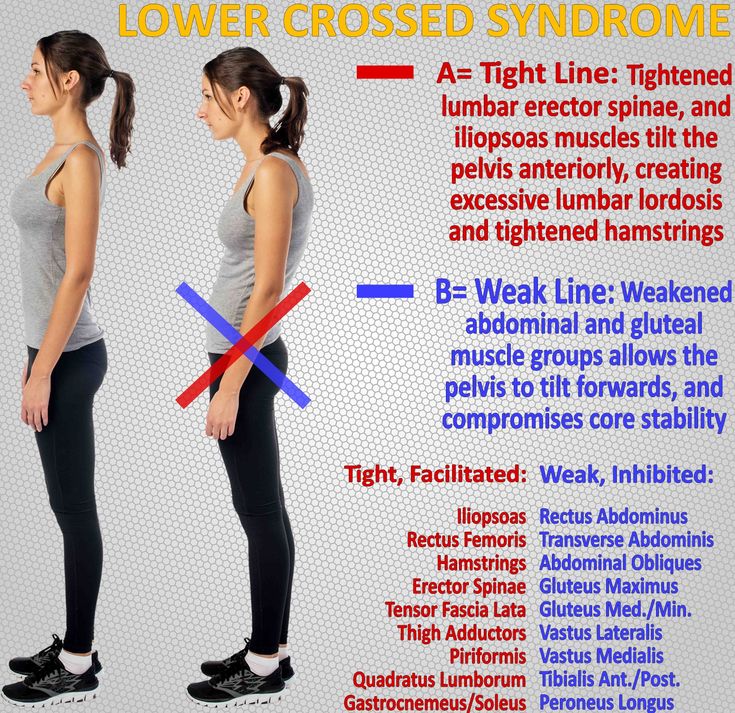
Since the psoas muscle cannot be seen or really even felt it is often neglected. Through lot’s of sitting (think school, watching television, or long drives to dance class) the iliopsoas shortens and if it not strengthened and lengthened it can not get stronger, so you are left with a tight and weak iliopsoas. A tight and weak illiopsoas can create an anterior pelvic tilt—>sticking your booty out. If the body is in anterior pelvic tilted position while dancing, it is NOT the optimal position to engage the abdominal muscles and glute muscles, or turnout muscles, so all aspects of your dancing suffer. Plus, since your body doesn’t have the iliopsoas doing its job correctly, other muscles will try to help out, which takes power away from them doing their own jobs correctly.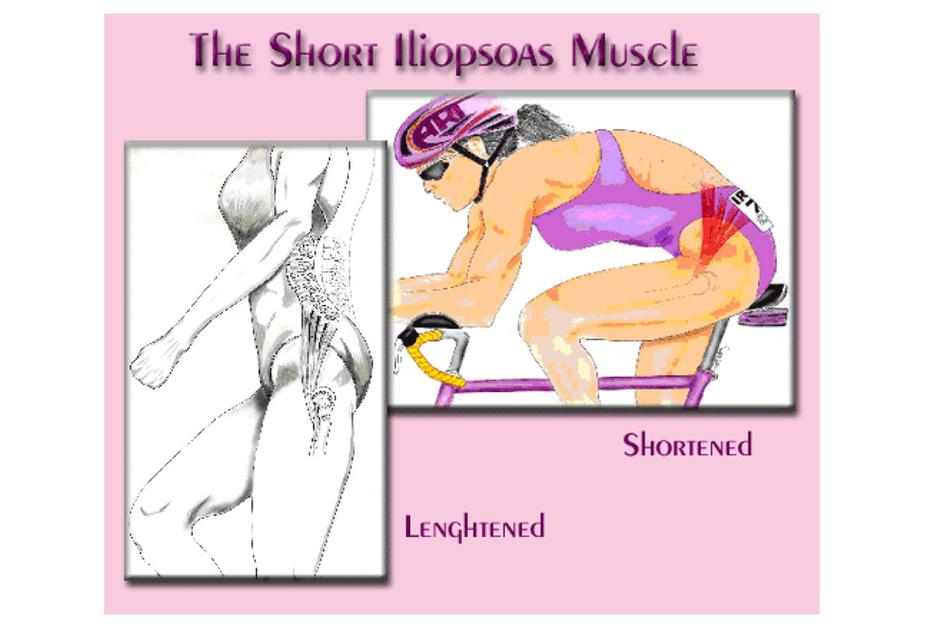
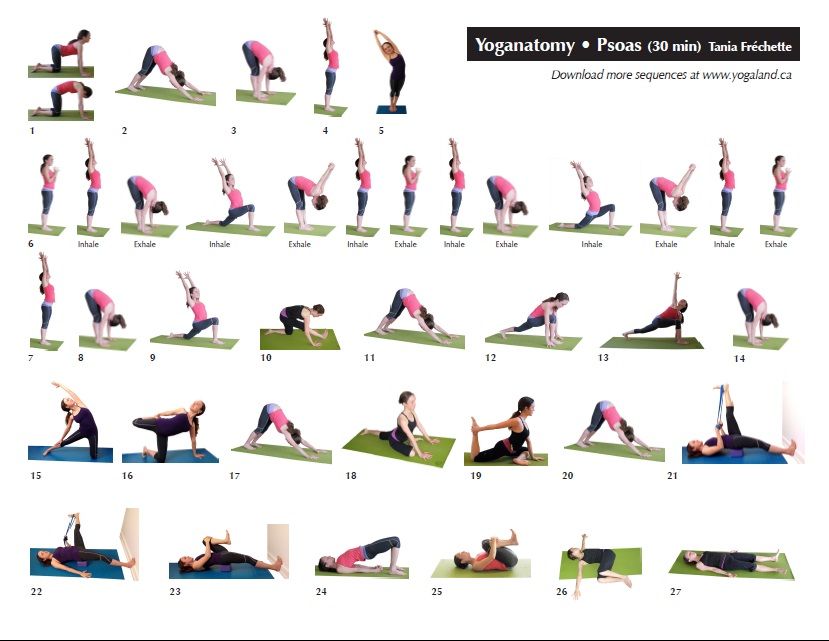
This is why dancers must STRENGTHEN AND STRETCH the iliopsoas muscle then learn to apply it to dance drills. Today I’m going to give you some strengthening and stretching exercises, and I will dive deeper into visualization of the iliopsoas through movement and applying these strength principles to dance drills later on!
Here are the iliopsoas exercises to get you started! With all of these exercises, visualize the placement of the muscle contracting while bringing your thigh closer to your chest. One visualization that has helped me is thinking of a pulley from my lower back, where the iliopsoas starts, to my knee, using the top part of the pulley to bring the knee up closer and closer to my chest. Sometimes placing one hand by part of the iliopsoas…a few inches below the belly button and a few inches to either side, can help bring an awareness to activating the muscle as well.
- Standing Hip Hold: Use hands to pull thigh as close as you can to your chest. Release the hands and hold the leg in place for 5-10 seconds.
 Repeat 4-5 times. [wpvideo do3I5bqr]
Repeat 4-5 times. [wpvideo do3I5bqr] - Hip Pulses: Sit on floor and bring one leg into your chest. Pulse the knee into your chest for 5-10 pulses, release and extend leg, then repeat 2-3X. [wpvideo FHd9fn8s]
- Standing Box Lift: Place one foot on a box tall enough that when lifting the knee it will come past parallel. Engage the iliopsoas and lift the thigh to the chest with control. Tap the foot down on the box and repeat 5-10X on each side. [wpvideo n6UZTES9]
- Illiopsoas Stretch: Place the back foot on an elevated surface behind you (if doing this at home a couch works perfectly and a wall works fine if you are at dance class), relax into the stretch while pulling the back hip forward into a deep stretch. Hold for 1-2 minutes on each side.
Have any questions on how to engage your iliopsoas or how you can become more Feis Fit?! Feel free to send me a message on Facebook or through the “Contact Us” section. Happy Feis-ing!
Strengthening the Iliopsoas for Higher, Pain-free Leg Extension
by Guest Contributors
Photo is courtesy Minnaa.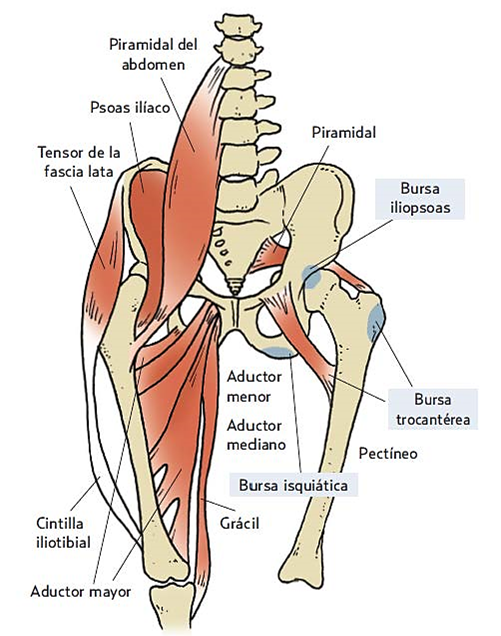
When I received Amy’s question about difficulty and pain in developpé below, I took her question to someone more knowledgeable than I on the subject. Deb Vogel is a neuromuscular educator and movement analyst who has been working with dancers for years. She is an author and columnist skilled at answering questions just like Amy’s. She’s has been kind enough to respond to our reader below.
Hello, my name is Amy. I recently stumbled upon your article regarding the psoas and it immediately sparked something inside. I am twenty years old and danced for majority of my life. I started ballet a little later than most around ten. I have been dancing with different ballet companies, but find myself still crying myself to sleep at night because I cannot get through a center exercise/adage with my terrible extension. I have had training growing up where there was no discussion or thorough understanding of HOW to lift one’s leg or what those muscles really do.
I have turnout and can kick quite high, but ask me to develop my leg past my knee and I cringe and tear up. (Sounds so dramatic, but hurts so badly). As I begin to lift I immediately feel the top part of my leg tense and it feels like someone is pushing down upon my leg as I go higher. I know that is not how the leg should be lifted. I cannot find any teachers to help me fix this issue, I have asked around and perhaps their discussions or explanations make no sense. I feel like no matter how much I try, I cannot fix this issue. I am desperate to at least be able to hold my leg a little above 90 degrees with ease. I figured perhaps, you might have a little insight that could point me in the right direction. Thank you so much for taking the time to read this, and I hope you can help!
Sincerely,
Amy
Here is what Deborah had to say to Amy:
Amy, you are on the right track with thinking that it might be a strength issue with the iliopsoas muscle.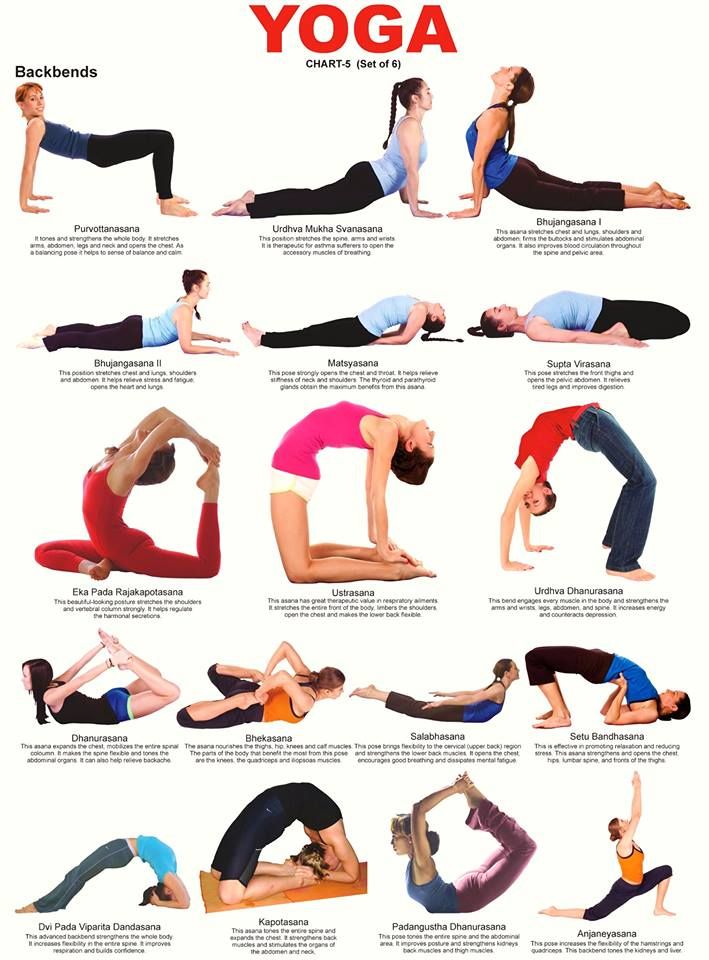 As Nichelle pointed out in her article on the iliopsoas – when the leg gets above 90 degrees the quadriceps lose their leverage and the iliopsoas becomes the prime mover of an extension. You would think that doing multiple grand battements and kicks in class would strengthen the iliopsoas – but they don’t.
As Nichelle pointed out in her article on the iliopsoas – when the leg gets above 90 degrees the quadriceps lose their leverage and the iliopsoas becomes the prime mover of an extension. You would think that doing multiple grand battements and kicks in class would strengthen the iliopsoas – but they don’t.
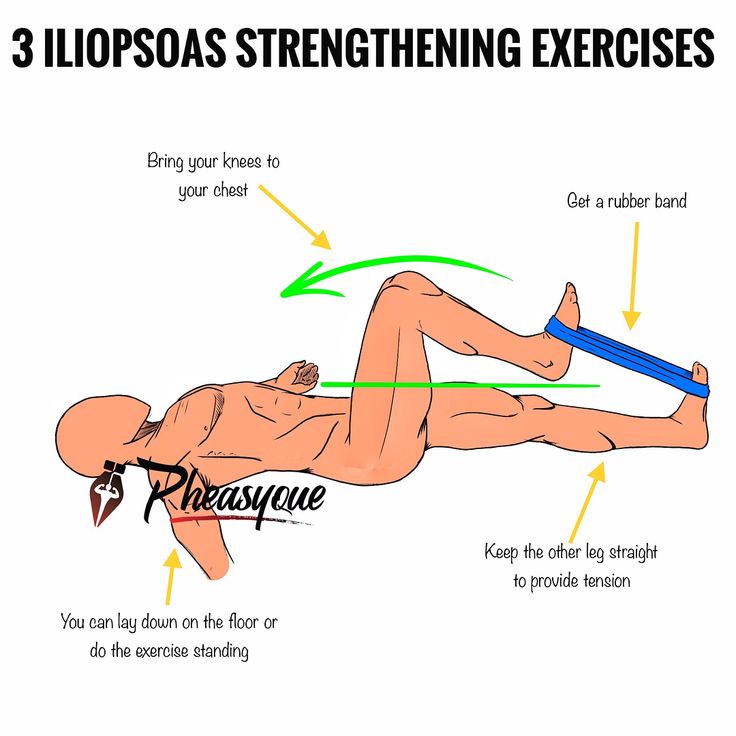
Here’s a simple and easy way to start strengthening your iliopsoas. Sit on the front part of a chair with your back long and tall, both feet on the ground. You are going to monitor staying on top of your pelvis – don’t let yourself roll to the back side of the pelvis during this exercise. Start by lifting one knee up towards the ceiling, and then lower it just so your toe touches, and lift it again. Can you do 20 repetitions without fatiguing? That would be your first goal, and you’ll be delighted at how quickly you gain strength.
Do the same movement on the other leg. If you want to make this more challenging you can tie a Theraband around both thighs to provide resistance to the leg that’s lifting.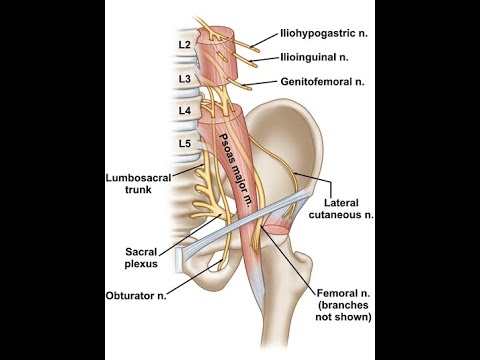
Once that becomes easier to do you can lean back in your chair so your back is against the back of the chair (your lower back and pelvis may be slightly tucked under, that’s okay for this exercise – even though it isn’t for your standing alignment). Now have one knee bent with your foot on the floor and the other leg straight. Turn the straight leg out slightly before lifting it up as high as is comfortable to the front before lowering to the level of the other knee. Continue lifting and lowering the straight leg up to 20 times before doing the other leg.
Another variation is to lift the leg up as high as you can, bend it into a passé like position and then straighten it forward (parallel to the ground). Then reverse, bending the knee and lifting the thigh like a developpe to the front and then lower the leg to parallel to the floor. You can again use the Theraband wrapped around the thighs to make it more challenging.
In the beginning, your iliopsoas may tire very quickly….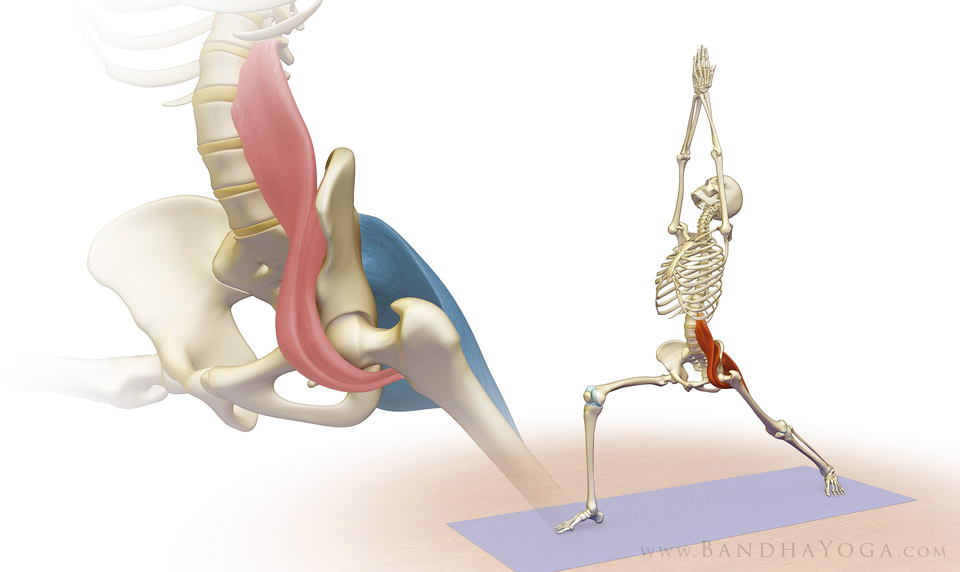 but in a relatively short time you will see improvement. It goes without saying that after you have spent some time strengthening the iliopsoas you would then want to stretch it out with doing one of the many variations of lunge stretching. I’ve put a short video up on YouTube on iliopsoas stretching.
but in a relatively short time you will see improvement. It goes without saying that after you have spent some time strengthening the iliopsoas you would then want to stretch it out with doing one of the many variations of lunge stretching. I’ve put a short video up on YouTube on iliopsoas stretching.
Hope that helps!
Deborah
Author, academic, and co-founder of The Center for Dance Medicine in NYC, Deborah Vogel has been involved in the medical field since 1978, helping hundreds of people – from dancers to athletes to office workers – get the most out of their bodies while minimizing injury risks. Her articles can frequently be found in Dance Teacher, Dance Spirit, and Pointe Magazines Deborah wrote Tune Up Your Turnout: A Dancer’s Guide, and has co-authored a 3-level guide for teaching functional anatomy in bite-size pieces within a class format. She offers a free newsletter for dancers on injury prevention and technique tips as well as running The Body Series, an online source of educational products for dancers and dance teachers.
Currently, she is on faculty at Oberlin College and the Oberlin Conservatory of Music.
Kindly follow, like or share:
Guest Contributors
Dance Advantage welcomes guest posts from other dance teachers, students, parents, professionals, or those knowledgeable in related fields. If you are interested in having your article published at Dance Advantage, please see the following info on submitting a guest post. Read posts from guest contributors.
Filed Under: Blog, Dancing, Health, Wellness & The Dancer's Body, Technique Tagged With: Anatomy, ballet, deb vogel, deborah vogel, developpe, extension, iliopsoas, kinesiology, movement analysis, question, stretching iliopsoas, the body, the body series
The simplest exercises for the most important muscle - Biomechanics of Flexibility
Biomechanics, Flexibility, New Articles, Exercises, Wellness
by YuliaGro
The psoas resembles a river with many streams, it originates from the lower thoracic vertebrae and is attached to the inside of the femur, and in fact connects the upper body to the lower.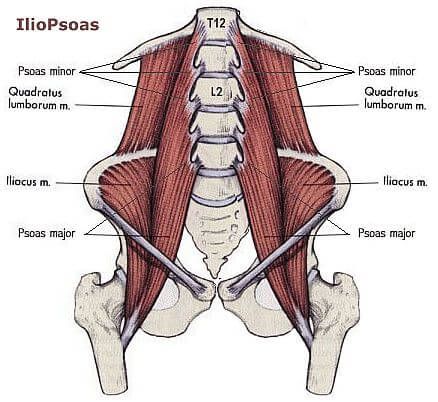 The health of your back, knees and ankle depends on its condition, it also affects the position of the internal organs, and hence their work. It is she who helps or prevents you from sitting on the splits and getting on the bridge - after all, we often deprive her of attention and create conditions in which she loses elasticity and strength.
The health of your back, knees and ankle depends on its condition, it also affects the position of the internal organs, and hence their work. It is she who helps or prevents you from sitting on the splits and getting on the bridge - after all, we often deprive her of attention and create conditions in which she loses elasticity and strength.
The psoas muscle has a true “partner” – the iliacus, it does almost the same work as the psoas, it is difficult to isolate their work. Their main difference is that the lumbar is able to raise the leg higher than 90 degrees, while the iliac muscle starts lower and, accordingly, higher than itself, it cannot pull the femur.
The second important moment in the work of the psoas muscle: it is connected with all the vertebrae of the lumbar . Let's do a little experiment:
- Stand up straight and lift your straight leg forward: in this position, the psoas muscle contracts, pulling the femur closer to the spine.
- Take the straight leg back: in this position, the psoas muscle is stretched, and if it is not elastic enough, then in this position you will have to bend the lower back more - the muscle will pull it along with it.
- Staying in this position, tighten your abdominal muscles, helping the spine return to its place, do not lower your leg, feel the tension increase in the front of the thigh. Meet your iliopsoas!
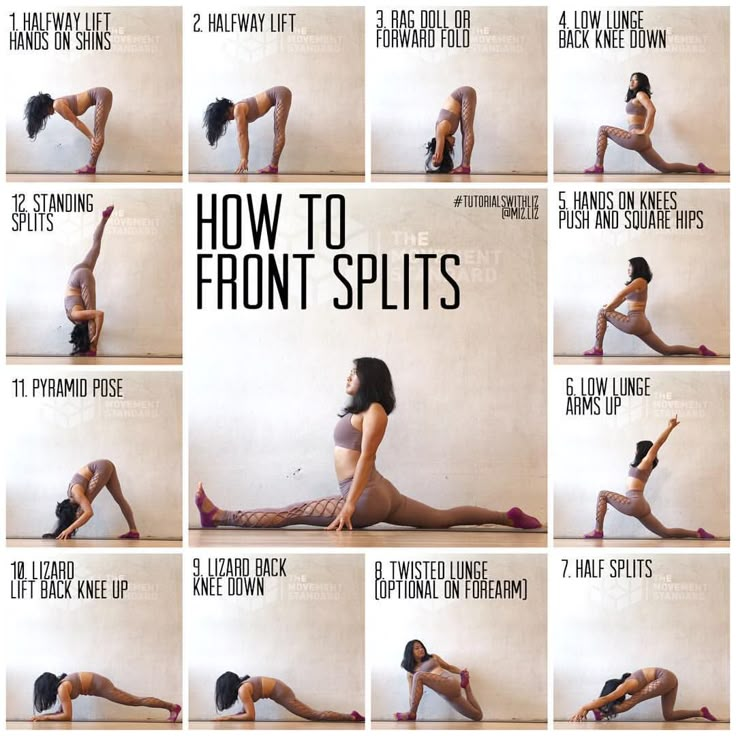
The psoas stretch is needed to bring the straight leg back. Have you seen girls who walk in heels without straightening their knees? (I'm talking about street walkers, not catwalkers.) A shortened psoas makes it difficult to straighten your leg while walking. Stretching it is not so difficult, there are many exercises, and thanks to this, the gait will become much more graceful.
This muscle also needs attention when you get up on the bridge. If it is not elastic enough, there will be discomfort in the lower back.
And, of course, it is precisely this elasticity that is often lacking for those who are trying to sit on the splits. A lot of people keep their body weight in front, sitting on their front foot, instead of paying more attention to the back. It is worth developing the psoas muscle well together with the iliacus, then the load on the front leg in the split becomes less, reducing the risk of stretching it.
A lot of people keep their body weight in front, sitting on their front foot, instead of paying more attention to the back. It is worth developing the psoas muscle well together with the iliacus, then the load on the front leg in the split becomes less, reducing the risk of stretching it.
A defect in the lumbar muscle threatens with problems with the back, as well as with the knees. Remember: non-extending legs when walking overload the knee joint over time. For the same reason, problems with the ankle are possible.
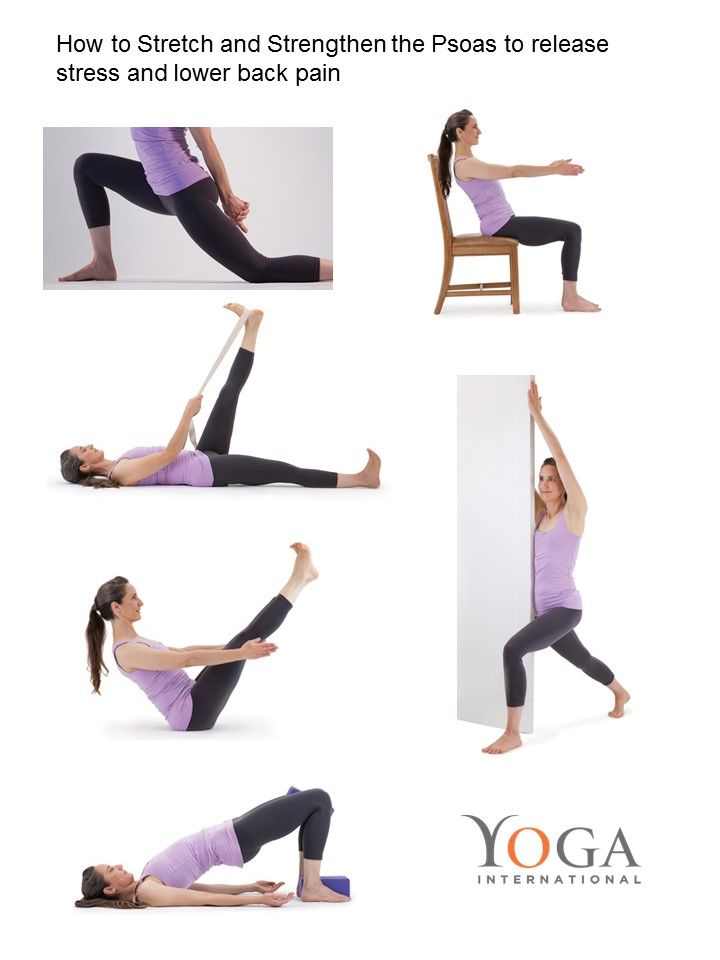
The psoas aligns us when we are looking for balance. Give it time and your body will move more balanced in every sense of the word. I picked up a few simple exercises to stretch and strengthen it, in fact there are a lot of them, and you can find various variations on the Internet if you type in the image search the expression “ psoas stretch ” - stretching the psoas muscle.
The psoas muscle is perfectly felt when moving a straight or half-bent leg back. Take care of your lower back, do not forget to hold it with your abdominal muscles. With your arms stretched up, continue to open your hips and try to pull your lower ribs as high as possible, lower your shoulder blades and shoulders down, and be sure to pull in your stomach. Another great stretching exercise. Watch your lower back and try to take your leg back precisely at the expense of the hip, and not the deflection in the back. The boat is an excellent exercise to strengthen the psoas muscle. I do not recommend it to owners of serious problems with the spine: it is VERY important to keep your back straight, not to bend, try to lengthen the spine and control its position with the help of the abdominal muscles. A more gentle option is suitable for those who find it difficult to keep their back straight in the previous exercise. Again, pay attention to the position of the body, there should be no deflection in the back!
Take care of your lower back, do not forget to hold it with your abdominal muscles. With your arms stretched up, continue to open your hips and try to pull your lower ribs as high as possible, lower your shoulder blades and shoulders down, and be sure to pull in your stomach. Another great stretching exercise. Watch your lower back and try to take your leg back precisely at the expense of the hip, and not the deflection in the back. The boat is an excellent exercise to strengthen the psoas muscle. I do not recommend it to owners of serious problems with the spine: it is VERY important to keep your back straight, not to bend, try to lengthen the spine and control its position with the help of the abdominal muscles. A more gentle option is suitable for those who find it difficult to keep their back straight in the previous exercise. Again, pay attention to the position of the body, there should be no deflection in the back! Like this:
Like Loading...
Tagged with: Flexibility balance biomechanics health health knowledge knees bridge leg muscles posture spine gait loin psoas muscle stretching back exercise twine You must log in to post a comment.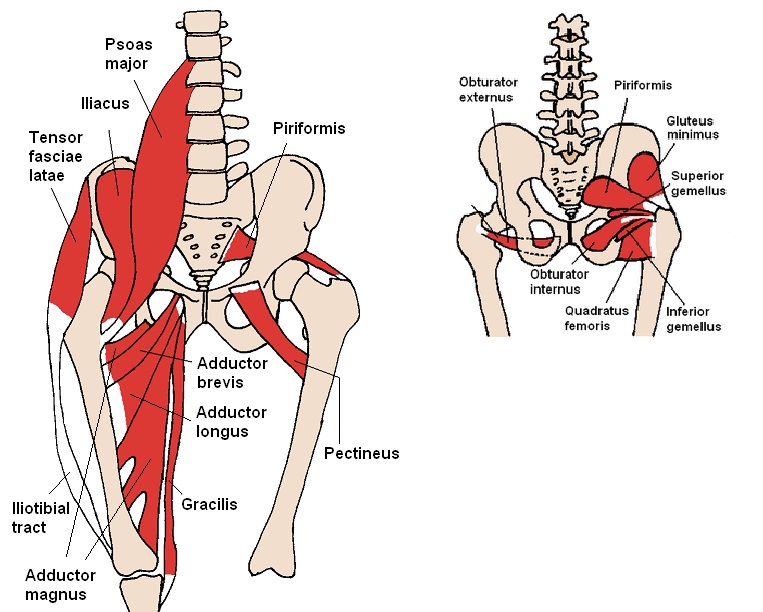
Iliopsoas syndrome (IPMS), myofascial iliopsoas syndrome, iliopsoas tendinitis
Iliopsoas syndrome (IPMS), myofascial iliopsoas muscle syndrome, iliopsoas tendinitis | Diagnosis and treatment of diseases and trauma of the hip joint Kyiv, Ukraine
Why is the iliopsoas often overlooked? How to understand that the pain is caused by her? Which doctor will help you? The iliopsoas muscle is one of the most unpredictable and insidious muscles in our body. Participating in almost all movements of the lower extremities and lower back, it often causes pain.
Published: 15.07.2022Iliopsoas muscle syndrome (IPMS), myofascial iliopsoas muscle syndrome, iliopsoas tendinitis.
Review of materials from open sources. Exclusively for the project "Traumatology and pharmacology: points of contact".
The promised continuation of a series of materials on pain in the hip joint in young patients under 40 years of age.
The iliopsoas muscle is one of the most unpredictable and insidious muscles in our body. Participating in almost all movements of the lower extremities and lower back, it often causes pain. At the same time, she manages to remain above suspicion and elude the attention of doctors. Because of this feature, she was nicknamed - "secret prankster" [J. Travell D. Simons. Myofascial pain and dysfunction. Volume II. S. 101].
Why is the iliopsoas often overlooked? How to understand that the pain is caused by her? Which doctor will help you?
Anatomy, symptoms, causes, diagnosis, treatment, rehabilitation and prevention of iliopsoas muscle syndrome.
1 and 2 psoas major and minor, 3 iliacus
Anatomy. A few words about the structure of the iliopsoas muscles
1. Iliopsoas 2. Ilium 3. Psoas major 4. Psoas minor 5. Tendon of psoas minor 6. Inguinal ligament 7. Pubic bone 7. Lesser trochanter 9. Femur
Pubic bone 7. Lesser trochanter 9. Femur
The iliopsoas muscle (IPM) complex consists of three muscles which include the iliacus, psoas major and minor muscles. The iliac muscle originates in the iliac fossa and attaches to the tendon of the psoas muscle and the lesser trochanter of the femur. The psoas major also inserts on the lesser trochanter of the femur and originates from numerous structures including the transverse processes of the lumbar vertebrae, intervertebral discs, and the margins of the vertebral bodies from Th22 to L5 and the tendinous arch. Finally, the psoas minor originates from the Th22 and L1 vertebral bodies and inserts on the iliopubic eminence and iliac fascia.
In some people, the psoas muscle is divided into 2 muscles: psoas major and psoas minor. The small psoas muscle is present in only 60% of people.
Psoas major and iliacus fuse at the level of L5-S2 vertebrae. Before attaching to the lesser trochanter, the RPM exits the pelvic cavity into the thigh region (under the inguinal ligament, where it crosses the anterior part of the acetabulum, between the anterior inferior iliac spine (laterally) and the iliopubic eminence (medially).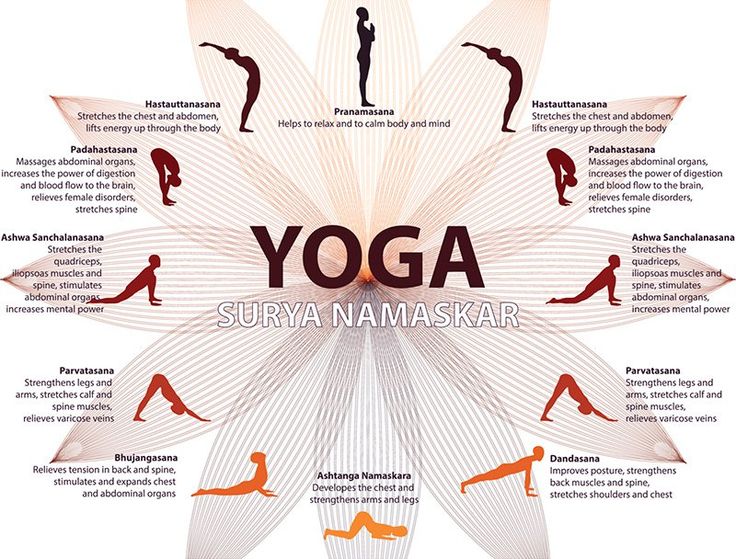 The largest bursa of the hip joint is iliopsoas bursa, which is located deep at the iliopsoas musculoarticular junction and anterior to the hip joint capsule.The bursa is thought to communicate with the hip joint in ~15% of patients.
The largest bursa of the hip joint is iliopsoas bursa, which is located deep at the iliopsoas musculoarticular junction and anterior to the hip joint capsule.The bursa is thought to communicate with the hip joint in ~15% of patients.
It is important to remember that it is attached to the lesser trochanter and is responsible for lifting the leg forward. Often, people mistakenly think that they are pumping the abdominal muscles (rectus abdominis), but in fact they overload and contribute to the formation of triggers in the iliopsoas muscle.
Innervation of the iliopsoas muscle
The psoas major muscle is innervated by branches of the lumbar plexus containing fibers of the spinal nerves L2, L3, L4. The psoas minor is innervated by a branch of the first lumbar spinal nerve. The iliac muscle is innervated by the spinal nerves L2 and L3.
The iliac muscle (IM) is located in the abdomen in the iliac recess. It is located deep enough, so it will not work to probe it. From above, it is attached to the upper two-thirds of the iliac fossa (depression on the inner surface of the iliac wing). It covers the anterior wall of the large pelvis, and then is fixed on the femur. The PM and tendon of the iliopsoas muscle at the outlet of the pelvis pass in the muscle gap along with the femoral nerve, as well as the lateral cutaneous nerve of the thigh.
From above, it is attached to the upper two-thirds of the iliac fossa (depression on the inner surface of the iliac wing). It covers the anterior wall of the large pelvis, and then is fixed on the femur. The PM and tendon of the iliopsoas muscle at the outlet of the pelvis pass in the muscle gap along with the femoral nerve, as well as the lateral cutaneous nerve of the thigh.
I would like to note this point - it is the deep and complex location of this complex that makes it difficult to diagnose pathological processes in it.
Due to the fact that the iliac muscle is located next to the femoral nerve in such a narrow opening, there is a risk of pinching of the femoral nerve if the femoral nerve is affected. Then pain and other unpleasant symptoms appear, which we have repeatedly described in the material on tunnel syndromes - nerve compression syndromes.
Functions of the iliopsoas muscle
The psoas remains active when the person is standing or sitting.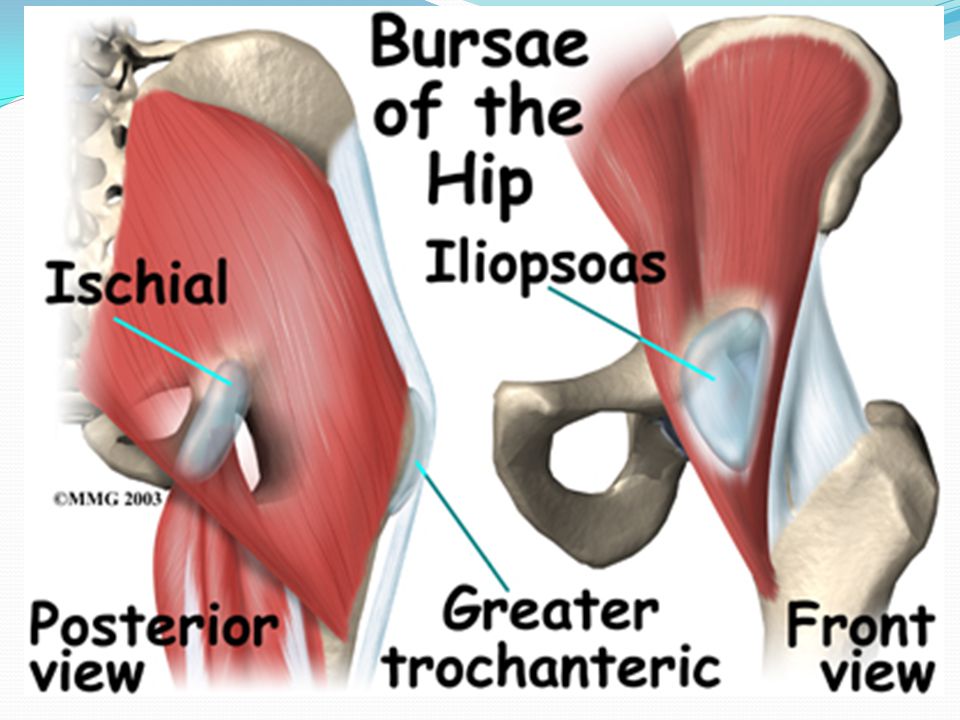 It helps keep the body in an upright position.
It helps keep the body in an upright position.
- is the main "tool" for hip flexion;
- serves as an attachment for the rest of the thigh muscles located in the lumbar region;
- is involved in movement and bending of the legs both in the thigh and knee area;
- allows you to press your knees to your chest;
- participate in external rotation of the hip;
- are involved in flexion and extension of the lumbar spine;
- are involved in pelvic movements;
- is indispensable in matters of coordination of the whole body.
Iliac muscle activity during standing is minimal. When a person walks, the PM is active, and the BPM is tensed only at the moment before the swing of the leg and during its movement forward. The iliac muscle is involved during running, when a person bends the leg in the hip area. Also, the complex is involved in the stabilization of the entire core during active movements - running, jumping, playing sports, dancing .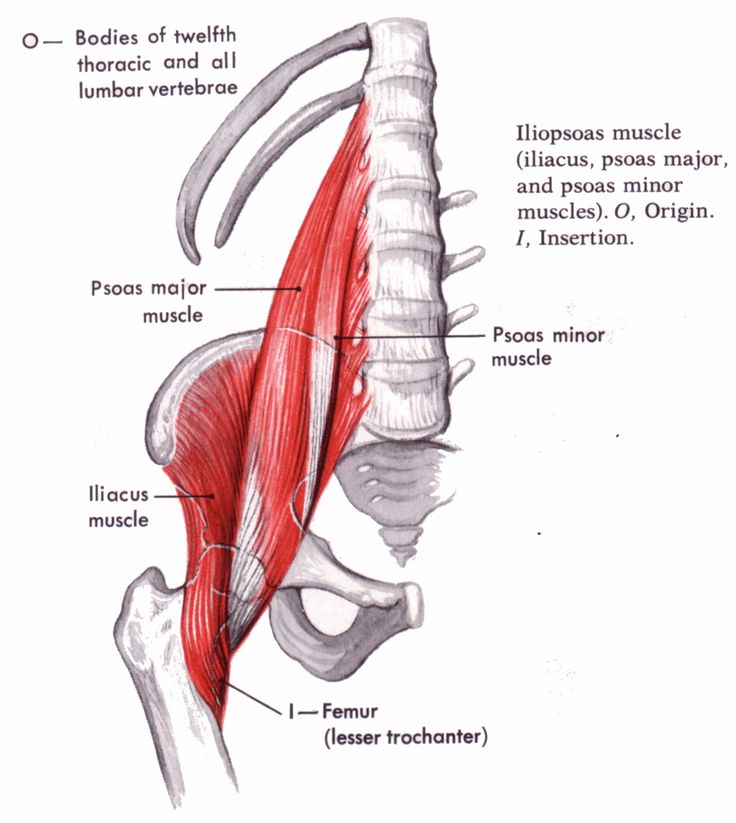 ..
..
PPM remains active when the person is standing or sitting. It helps to keep the body upright
This muscle has a direct connection with the deep muscles of the back. The condition of the entire back, in particular, the spine, depends on her health. One of the key muscles of the human body - the muscle that straightens the spine - is highly dependent on the hip joint and lower back. Consequently, at the advanced stage of diseases of the iliopsoas muscle, the deep muscles of the back also cease to function adequately, which often leads to such serious consequences as curvature of the spine and pelvic tilt.
Weakening of the RPM may cause slouching or contribute to the formation of a "flat back". When the back of the hip joint (HJ) is pulled, the hips are stretched. Normally, the PPM provides support and counteracts the tension that occurs. With stoop, the ligaments of the anterior part of the hip joint are in a stretched state for a long time, which can lead to joint instability.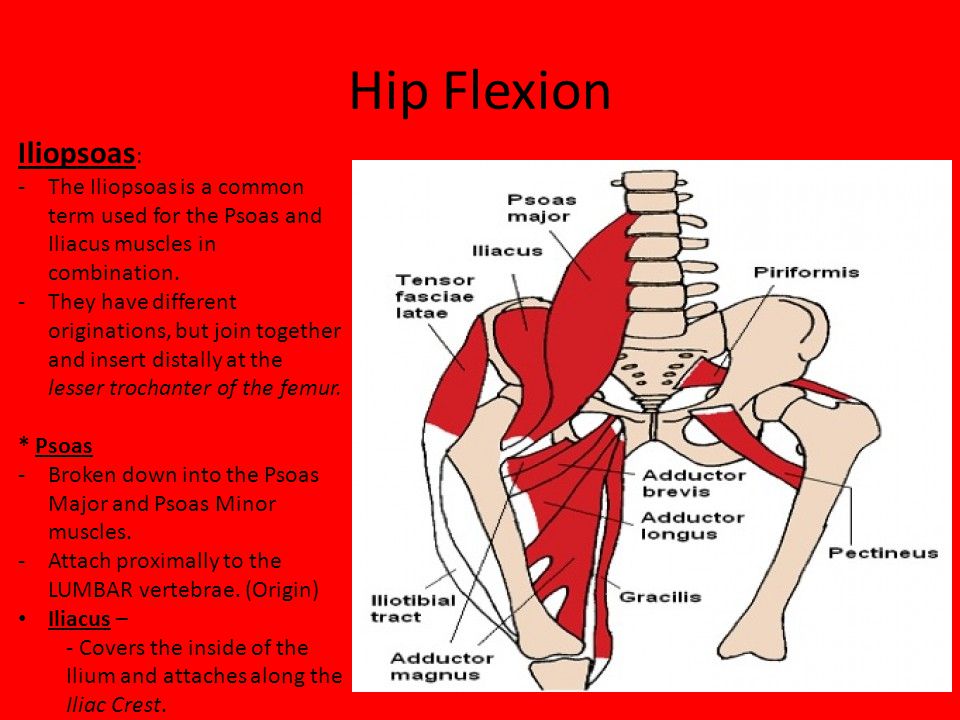 Due to excessive tissue compensation, the likelihood of muscle imbalance (violation of symmetry, mismatch in size and strength of paired muscles) increases.
Due to excessive tissue compensation, the likelihood of muscle imbalance (violation of symmetry, mismatch in size and strength of paired muscles) increases.
Symptoms of PPM damage
In case of iliopsoas muscle syndrome, the body often warps in the direction of the damaged organ. Then the load on the bone joints in the pelvic region increases. This inevitably leads to damage to the joint, as well as limited mobility, when the patient cannot fully flex / extend the limb. Such a condition can put the patient out of action for a long time, since any active movements are limited and bring pain .
SPPM has a pronounced clinical picture:
- The area of the hip joint begins to hurt when trying to make flexion/extension/rotation movements of the leg. Painful sensations can spread to the front of the thigh, lower back, and sometimes to the lower abdominal cavity. The muscles of the injured limb become weak, heaviness appears during movements, for example, when bending the hip or raising a straight limb.
- With a sharp movement of the leg, a sharp pain (lumbago) appears in the lumbar region.
- It is difficult for the patient to sit up from a lying position, often for this he needs the help of others or leaning on a wall or headboard.
- It is difficult for the patient to move without a cane, crutches. In the absence of assistive devices, he tries to lean on walls or furniture.
It is this unpredictable irradiation that often baffles the doctor and makes it difficult to find the culprit of pathological processes.
If the patient continues to self-medicate and does not turn to specialists, the pain in the thigh area increases, there is a feeling of numbness, tingling, and motor activity is greatly reduced. Since the femoral nerve is located next to the RPM, the risk of its compression is very high, when this happens, neuralgic disorders appear (numbness in the groin area, limbs, loss of the ability to sit down, lie down, stand up, etc. ). It becomes difficult for the patient to walk due to discomfort and pain.
). It becomes difficult for the patient to walk due to discomfort and pain.
Etiology and causes
Iliopsoas tendinitis is a structural change in the normal architecture of the tendon that is thought to be the result of microtrauma resulting from chronic overuse. Although the exact etiology of this condition has not been fully established, the two most commonly reported causes of ACL tendon irritation involve either acute injury or overuse injury.
- Acute trauma is less common but may result in musculoskeletal injury or avulsive fracture of the lesser trochanter. This usually occurs as a result of an eccentric contraction of the muscle or a sudden flexion against a tensile force that is greater than the tendon's capacity.
- Excessive ATM injuries can result from any activity that requires repetitive hip flexion, repetitive external rotation, or repetitive flexion of both the hip and trunk.
Some examples of activities that may predispose people to APM injury include ballet, cycling, rowing, running, athletics, football, and gymnastics.
Sometimes there is another reason - a metabolic disorder in tissues, it is associated either with infectious (sometimes with autoimmune) diseases or genetic disorders.
In general, PPM pathological conditions such as tendonitis, bursitis, clicking and impingement are considered to be the main cause of chronic groin pain in approximately 12-36% of athletes and in 25-30% of athletes with acute groin injury.
Causes and risk factors
- Hypothermia of the lumbar region, legs. It can be a long stay on a cold street in out-of-season clothes. Often suffer after sitting in a draft, for example, from the air conditioner in the summer. Risk factor - swimming in the heat in a cool pond. Swimming in cold water or diving into the snow after sauna.
- Poisoning, including alcohol or drugs.
- Excessive exercise. Physical injuries or blows to both the lumbar region and the buttocks, thighs. Even an impact that does not leave an external manifestation can lead to muscle spasm, swelling, strangulation of fibers, and internal hematomas.
- Problems with vessels and circulatory system.
- Infectious diseases.
- General weakening of the body due to autoimmune diseases and other immune disorders.
- Systematic use of hormonal drugs.
SPPM Diagnostics. Specific functional tests and hardware diagnostics
As usual, any diagnosis begins with taking an anamnesis: find out possible causes, injuries, time of onset of the first symptoms, etc.
You can notice the symptoms of STDs by moving the spine forward. Then, when bending the leg, the lower pairs of ribs stick out. It is difficult to do this while walking, so it is better to take a horizontal position. To perform this test, lie on your back, bend your knees, and lift your thighs off the floor. If in this position the lower ribs bulge, then this indicates SPPM.
The following investigations are ordered to detect STDs that are accompanied by pain:
- X-ray in two projections shows that the density of the iliopsoas muscle is increased.
 In addition, the picture shows the pelvic tilt and associated excessive deflection in the lower back (hyperlordosis).
In addition, the picture shows the pelvic tilt and associated excessive deflection in the lower back (hyperlordosis). - With the help of magnetic resonance imaging, it can be seen that the contour of the psoas muscle in the region of 2-4 vertebrae is enlarged, most likely due to its increased tone.
- Needle electromyography is used to detect involuntary activity in the joints of the pelvis and hips.
- Sometimes, with an unclear picture and suspicion of another pathology, laboratory tests may be prescribed. Clinical analysis of blood and urine, as well as the determination of erythrocyte sedimentation rate, C-reactive protein, rheumatoid factor, antibodies to cyclic citrullinated peptide and antinuclear antibodies. These tests are useful in looking at pathology of the abdomen and pelvis, which can present as groin pain due to colon cancer, diverticulitis, prostatitis, salpingitis, kidney stones, appendicitis, and psoas abscess.
SPPM and associated unilateral or bilateral pelvic pain can be diagnosed with a specific test.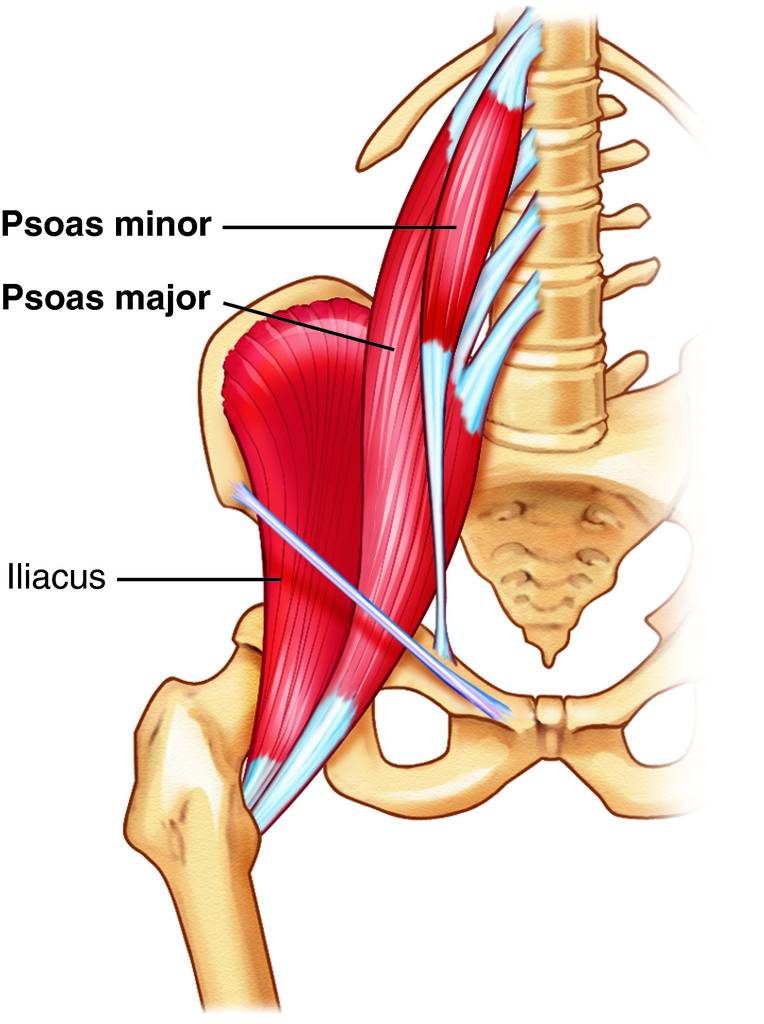 To do this, the patient lies on his back, bends his leg at the knee, then with the palms of both hands, presses on the knee and alternately (for 10 seconds) strains and relaxes the limb for 3 minutes. The movements must be repeated for the other leg. If after performing the test, pelvic pain is relieved, then this indicates MTSS.
To do this, the patient lies on his back, bends his leg at the knee, then with the palms of both hands, presses on the knee and alternately (for 10 seconds) strains and relaxes the limb for 3 minutes. The movements must be repeated for the other leg. If after performing the test, pelvic pain is relieved, then this indicates MTSS.
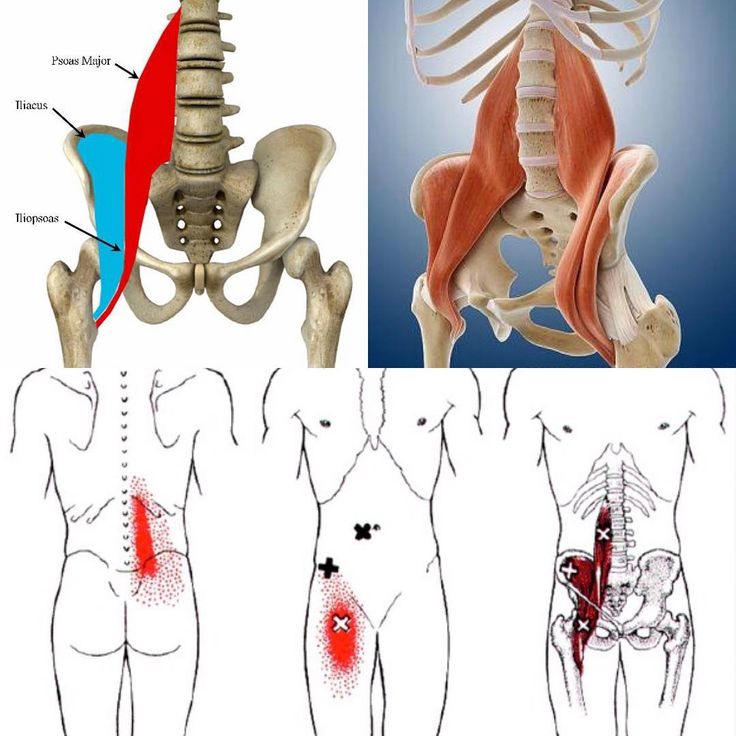
Extension of referred pain (bright red) on palpation of myofascial trigger points (X) in the right iliopsoas muscle (dark red). The essential pain zone is colored solid red, the diffuse pain zone is indicated by red dots. Increased pain on palpation of trigger points helps in making a diagnosis.
To check the status of the MRP, you can perform the following additional tests:
Thomas test
The patient stands at the edge of the table with his back to him, one knee and hip bent, the patient pulls them as close to the stomach as possible. Then he lies back so that the tailbone is as close to the edge of the table as possible, while avoiding lordosis.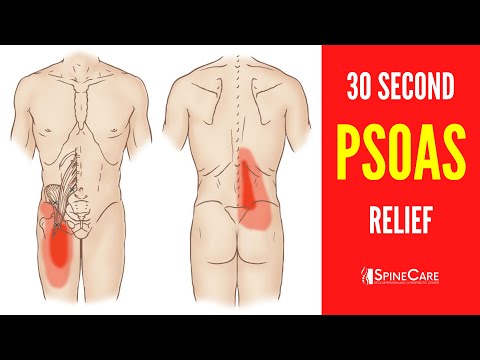 The second thigh should lie freely on the table. If this does not happen, the psoas muscle is shortened and is in good shape due to pathological processes in it.
The second thigh should lie freely on the table. If this does not happen, the psoas muscle is shortened and is in good shape due to pathological processes in it.
1. Positive test - there is a possibility of STD 2. Negative test
Two hand test. To assess the condition of the psoas muscle, place the edge of one hand on the upper chest, and the other - perpendicular to the pubic bone. Then you need to bend the body to assess the angle between the planes, in a healthy person they should be parallel to each other.
Trigger points - the presence of characteristic pain, burning, paresthesia, numbness, goosebumps at trigger points helps in making a diagnosis.
Ludloff sign (isolated assessment of the strength of the PPM): the patient is in a sitting position on the couch with legs extended, he needs to tear the heel of the affected leg off the table. The test is considered positive if muscle weakness and/or pain symptoms appear.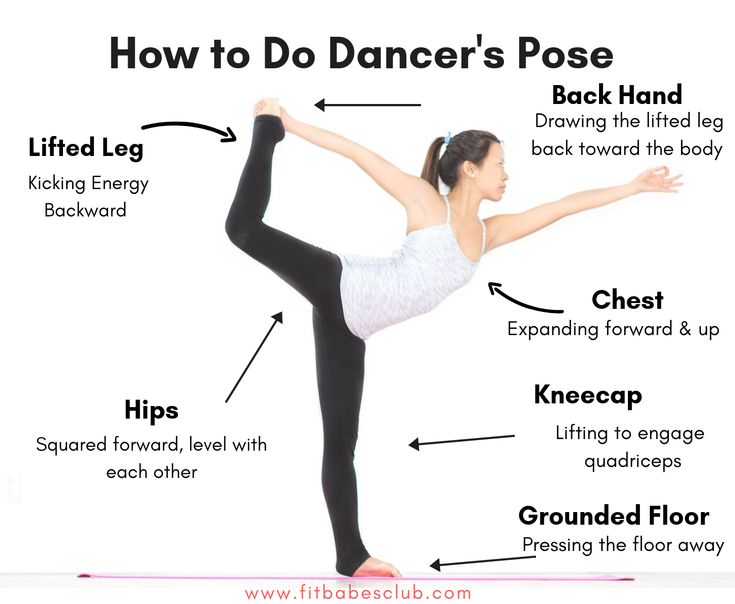
Stinchfield test: the patient performs an active straight leg raise to 45 degrees. He then needs to resist the downward force that is applied to the front of the thigh. Pain and/or muscle weakness indicate damage to the psoas muscle or intra-articular pathology.
Hip-click maneuver : The affected hip is in flexion, abduction, and external rotation. The hip moves passively into extension and internal rotation. A positive test is a palpable or audible click localized in the groin. Pain caused by this maneuver may be indicative of tendinitis or bursitis of the RPM.
If the MTSS is at an advanced stage, then it can be detected immediately after palpation.
Differential diagnosis. What not to confuse.
- Hip lip rupture.
- Sports hernia.
- Bursitis PPM.
- Inguinal hernia.
- Osteitis of the pubic bone.
- Abdominal tendinopathy/stretching.
- Hip adductor tendinopathy/groin injury.
- Osteoarthritis of the hip joint.
- Obturator nerve lesion.
- Neoplasm (cysts, oncology, chondromatosis).
- Osteonecrosis of the femoral head.
SPPM hardware imaging
X-ray diagnostics
- Generally not indicated for soft tissue disease, however, radiography may be used as an initial investigation if other bone pathology is suspected (eg, loose bodies, osteonecrosis, osteitis pubis) or if red flags are present.
- Displacement of the epiphysis of the femoral head should be excluded in a child or adolescent with hip pain.
Ultrasound diagnostics SPPM
- Ultrasonography (ultrasound) is a non-invasive and affordable method for evaluating muscle and tendon injuries. In this case, tendon thickening is usually found.
- PPM bursitis is associated with excess fluid in the iliac bursa, which is usually seen on ultrasound.

- Ultrasonography allows for dynamic assessment of the muscle, and therefore will reveal any tendon 'snapping' that may be present in these patients.
- Ultrasound is used to guide the needle for injections of lidocaine and corticosteroids in the diagnosis and treatment of
- Not always the best diagnostic method, since its accuracy is highly dependent on the skill of the specialist.
Magnetic resonance imaging SPPM
- MRI is now the "criteria" or, as we have repeatedly called it, the "gold standard" for assessing hip and pelvic symptoms. One study that looked at imaging to determine the cause of hip pain compared radiographs, radionuclide bone imaging, and MRI. The results showed that MRI is the most sensitive imaging modality.
- Provides the most accurate evaluation of the PRM tendon and bursa.
MRI results for assessing musculotendinous injuries:
- T2-weighted spin echo images will show increased signal intensity associated with swelling and inflammation.
 Severe musculotendinous injury with concomitant hemorrhage will have high signal intensity with both T1-weighted images and T2-weighted images.
Severe musculotendinous injury with concomitant hemorrhage will have high signal intensity with both T1-weighted images and T2-weighted images. - Peritendinitis Evaluation - Peritendinous tissue will display increased fluid content, which is found on T2 spin echo-weighted images or short sequence T1 inversion recovery (STIR) as a focus of high signal intensity surrounding the normal tendon.
- Tendinosis spin echo T1-weighted images show increased signal intensity in the tendon, which is associated with myxoid degeneration or angiofibroblastic proliferation. Spin echo T2-weighted images may show an abnormal signal (usually less than T1-weighted images) or a normal signal.
MRI provides almost 100% confirmation of most pathological changes in the PPM, but a highly professional ultrasound doctor will be able to confirm the diagnosis with a high degree of probability during an ultrasound examination. Such a specialist works in ITO NAMSU: Lyudmila Ivanovna Klimchuk - doctor of ultrasound diagnostics of the highest category, 20 years of experience.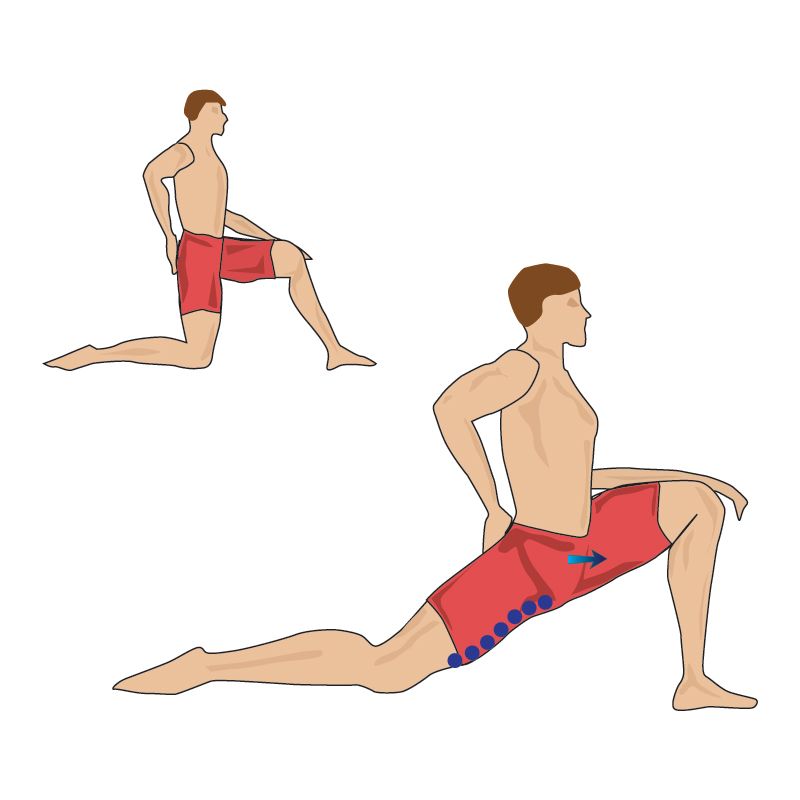
Lidocaine injections
It is necessary to inject lidocaine into the tendon of the PRM under ultrasound guidance. If a reduction in pain is achieved after the injection, then the diagnosis of myofascial iliopsoas muscle syndrome is confirmed.
Methods of treatment of STPM
The choice of treatment for SSPM depends on the stage of pathology. At an early stage, post-isometric relaxation is shown (restoring the normal tone of spasmodic muscles with the help of special exercises), if it is ineffective, the doctor will prescribe a therapeutic blockade.
PIR (post-isometric relaxation) is carried out under the supervision of a specialist. At home, to stretch the iliopsoas muscle, you can perform special stretching exercises. A rehabilitation specialist or exercise therapy doctor will tell you about these exercises and teach you how to perform them.
Drug blockade is prescribed to relieve severe pain in STPM. During the procedure, a solution of Novocaine, Hydrocortisone and cyanocobalamin is injected into the pain site.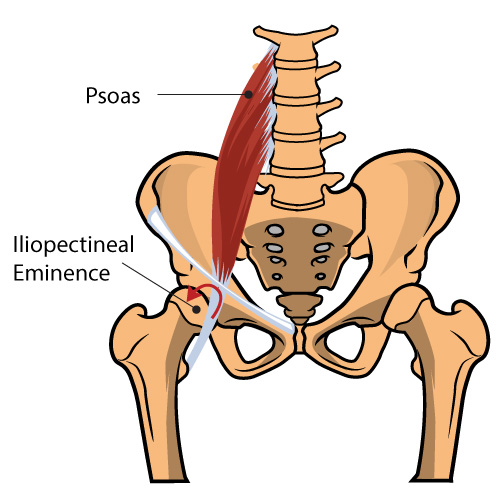 This procedure should be carried out only by a doctor in a medical institution with experience in performing this procedure and always under ultrasound control!
This procedure should be carried out only by a doctor in a medical institution with experience in performing this procedure and always under ultrasound control!
The following methods can be used to relieve spasm:
- Taking medication during an acute period prescribed by a doctor.
- Reflexology (acupuncture).
- Lumbar and thigh massage (by a professional or on your own).
- Warm bath or shower.
- Biomechanical or kinesiology taping of the hip joint for reflex relief of pain and improvement of trophism
Photos for beauty )))) The technique of taping PPM with PPM is completely different. Details can be obtained from Andrey Kif.
In addition, the patient must perform special exercises to strengthen and increase the elasticity of the PPM. Exercise therapy will help restore blood circulation, relieve spasm, restore tone. However, before training, you should consult with your doctor.
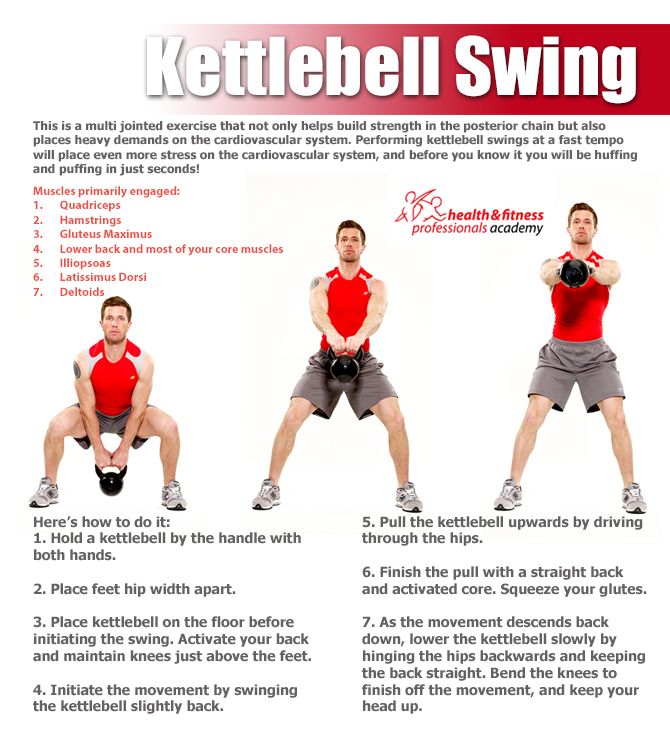
The following exercises will help strengthen the iliopsoas muscle:
- Lie on the couch, bend the injured leg at the hip and knee, and move it to the side as far as possible. Hang your shin off the sofa, then bend the other limb (as well as the first leg) and move it to the side. Press your lower back against the surface, fix in this position for 20 seconds.
- Roll over on your stomach (on the floor), put your hands on the surface, arch your upper body (above the waist). Then begin to pull up your neck and lift your head. Without changing position, take 20-30 smooth breaths. Then return to the starting position and relax.
- Roll over onto your back, press down on the floor, bend your knees, lift them up. Try to raise them as high as possible, if there is pain, then lower them a little, gradually increasing the height. Repeat 8-10 times.
These exercises can be done one at a time or you can choose one of them. They allow you to normalize the tone of the iliopsoas muscle and perfectly complement complex therapy.
They allow you to normalize the tone of the iliopsoas muscle and perfectly complement complex therapy.
Important! When performing exercises, you should carefully monitor your condition. If you feel unwell, the session should be stopped.
It is also necessary to follow a number of simple rules when performing the complex:
- all exercises should be performed slowly, without sudden movements and without excessive effort,
- breathing should be even and correct, without interruptions and delays,
- you should not perform exercises through force and before the onset of overwork.
ATTENTION! Before self-study, be sure to visit a doctor to confirm the diagnosis. It is the complexity of the differential diagnosis of this pathology with other possible diseases that makes it so insidious. If instead of STPM you have, for example, the initial stage of aseptic necrosis of the femoral head, or chondromatosis, by your actions you can harm the joint, which will lead to the development of coxarthrosis and the need for arthroplasty in the near future!
SPPM is one of the main causes of pain in the lumbar region, as well as the hip.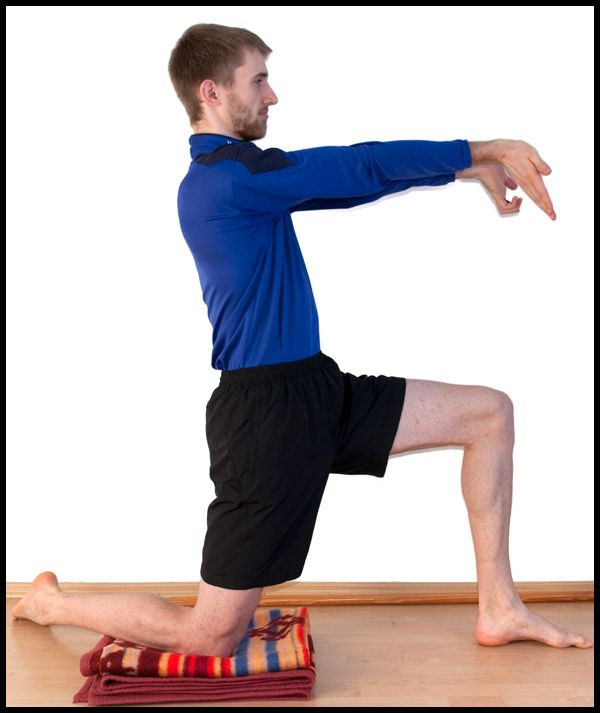 This condition requires complex treatment: medications, PIR, therapeutic blockades, exercise therapy, etc. If left untreated, the likelihood of serious complications, such as pinched femoral nerve, increases. Therefore, if discomfort, pain occurs, you should immediately consult a doctor who will conduct a thorough diagnosis and draw up a treatment plan.
This condition requires complex treatment: medications, PIR, therapeutic blockades, exercise therapy, etc. If left untreated, the likelihood of serious complications, such as pinched femoral nerve, increases. Therefore, if discomfort, pain occurs, you should immediately consult a doctor who will conduct a thorough diagnosis and draw up a treatment plan.
Operative treatment of SMPS
- Surgery is considered only when conservative treatment fails and the condition progresses
- Two surgical methods are described in the literature, which involve either complete or partial release of the RTM tendon and nerve decompression. Both options have good results, including pain reduction and no residual weakness.
SPTA Rehabilitation
Acute phase
- The main goal of the first phase is to reduce pain symptoms, muscle spasm and swelling. If the patient has ceased to engage in daily activities, then returning the patient to these activities is also an important goal of this phase.
- Rehabilitation in the acute phase includes relative rest (avoidance of any painful activity), use of cold, medication, and light stretching.
- Ice: exposure time 20 minutes, apply every 2 hours for the first 1-3 days.
- Drug treatment: short-term course of non-steroidal anti-inflammatory drugs (NSAIDs).
- Gentle stretching helps reduce muscle spasm. To avoid overstretching, do not stretch immediately after using the cold, as Local hypothermia can increase a person's pain threshold, making them less sensitive to pain.
- RPM stretch for 20 seconds, then 30 seconds of rest, repeat 5 times. Stretching should be painless, this can be combined with breathing phases.
Recovery phase
- The main goal of the second phase is to restore range of motion, strength, endurance and proprioception. After all, sports-specific activities are also included here.
- Range of motion: along with stretching, it is necessary to perform a warm-up and a cool-down.
- PLM injury may be associated with increased lumbar lordosis and anterior pelvic tilt. Achieving a neutral posture can be achieved by both stretching and strengthening the relevant muscle groups.
- Stretch:
- Stretching the rectus femoris helps bring the pelvis into a more neutral position. This will take the pressure off the PPM, reducing the chance of tension or spasm.
- All stretches in this phase are done as described in the acute phase (hold for 20 seconds, relax for 30 seconds, repeat 5 times).
- Reinforcement:
- Increasing the strength of the hamstrings increases the force exerted on the pelvis from behind and reduces the tension of the RPM pulling the pelvis forward.
- Abdominal strengthening exercises should be performed with the knees and hips bent to 90 degrees to allow the RMP to relax and the pelvis to remain in a neutral position.
- Strengthening the gluteal muscles also plays an important role in achieving a neutral pelvic position.
- Strengthening exercises performed daily (4 sets of 10-15 repetitions).
- Endurance training:
- An increase in RPM endurance can be achieved with repetitive movements (hip flexion or hip external rotation) performed with low resistance. Some examples include cycling, walking, climbing stairs.
- Endurance exercise should not cause pain, and there should be sufficient rest between endurance workouts. In the end, a person should exercise daily, gradually increasing the duration of activity.
Maintenance phase
- Continue stretching the RMB and rectus femoris.
- Gradually increase the load using resistance exercises (eg, seated RPM strengthening with ankle weights, supine hip lift, seated external hip rotation with weights or elastic band).
- RPM and Hamstring Strengthening Exercises - Gradually progressive resistance can be achieved either by increasing the number of repetitions performed or by increasing the weight (all individually).
 For example, standing hip flexion (machine), prone and seated knee flexion (machine), step up lunges (lunges are performed at a slower pace, providing a smooth and controlled rhythm).
For example, standing hip flexion (machine), prone and seated knee flexion (machine), step up lunges (lunges are performed at a slower pace, providing a smooth and controlled rhythm).
Return to normal life
- The patient must be asymptomatic or able to tolerate pain before considering returning to normal activities and sports.
- The range of motion, flexibility and strength of the hip flexors and antagonist muscles must be restored to the level of the contralateral side.
Forecast at SPPM
- Provided that the main biomechanical deficit is corrected, the overall prognosis is favorable.
- Early detection of this deficiency may play a role in preventing the development of chronic symptoms. However, as mentioned earlier, self-medication and an incorrect diagnosis can make the situation chronic and lead to compression of the nerve and surrounding tissues. In these cases, recovery may be delayed.
- The patient should not return to sports and their usual active lifestyle until they have achieved a full and pain-free range of motion.
Prevention of lumboiliac muscle syndrome
Prevention of inflammation of the iliopsoas muscle is to follow simple rules:
- watch your posture;
- take time to stretch the psoas;
- properly organize the place of work;
- avoid overload and hypothermia;
- contact a specialist in time;
Diseases of the knee, ankle, foot, flat feet and uncomfortable shoes can have a pathological effect on the biomechanics of walking. Which, in turn, can cause the PPM to be reloaded and damaged.
Conclusion
!!! Any pain in the back, hip joint, groin or thighs should be the reason for a mandatory visit to a doctor, because only a specialist can diagnose and prescribe a competent treatment that will help you return to a full life!!!
Specialists and clinics to help you with the diagnosis, treatment and rehabilitation of iliopsoas syndrome (IPMS)
Mikhail Polulyakh - Doctor of Medical Sciences, Professor, Orthopedic Traumatologist of the Highest Category, Honored Doctor of Ukraine
- Address:
- 01601 Kyiv, st.
 Bulvarno-Kudryavsaka, 27
Bulvarno-Kudryavsaka, 27
5th floor of the main building (left wing)
Contacts:
+38 (067) 731-53-13
+38 (044) 486-80-56
https://ortho.in.ua/
Working hours:
- Monday - Friday from 9:00-17:30
Consultation days: by appointment
Lyudmila Ivanovna Klimchuk - Doctor of ultrasound diagnostics of the highest category, ultrasound of the musculoskeletal system
- Address:
- Kiev, Chekhovsky lane, 7, ITO Polyclinic, 3rd floor, room. 315
Contact:
+38 (044) 486 36 36
+38 (050) 463 05 05
+38 (098) 999 31 22
Consulting days: by appointment
Andrey Kifa Rehabilitologist, specialist in kinesiology and biomechanical taping, physical rehabilitation
- Address:
- st.